Gastric Bypass Surgery
Gastric bypass surgery is one of the most effective and long-established procedures for long-term weight loss and metabolic health improvement. At Aurora Bariatrics, we offer two types of bypass procedures: Roux-en-Y Gastric Bypass (RYGB) and One Anastomosis Gastric Bypass (OAGB) — also known as Single Anastomosis or Mini Bypass. While the recovery, benefits, and post-operative care are similar, there are key differences in how each procedure is performed.
What is Gastric Bypass Surgery?
Gastric bypass is a weight loss procedure that reduces the size of your stomach and reroutes part of your digestive system to:
- Restrict how much you can eat
- Reduce calorie absorption
- Improve blood sugar control and hunger regulation
Both procedures are performed via laparoscopic (keyhole) surgery, involve creating a smaller stomach pouch, and bypass part of the small intestine. These changes not only support weight loss but also bring about powerful hormonal effects that help reverse obesity-related conditions.
Who Is It For?
Gastric bypass may be recommended if:
- You have a BMI > 40, or >35 with health conditions like Type 2 diabetes, sleep apnoea, or reflux
- You’ve tried diet, exercise, and medications without long-term success
- You suffer from severe gastro-oesophageal reflux and are not suited to gastric sleeve surgery
- You require revisional bariatric surgery
Our team will guide you through your options based on your medical history, goals, and current health.
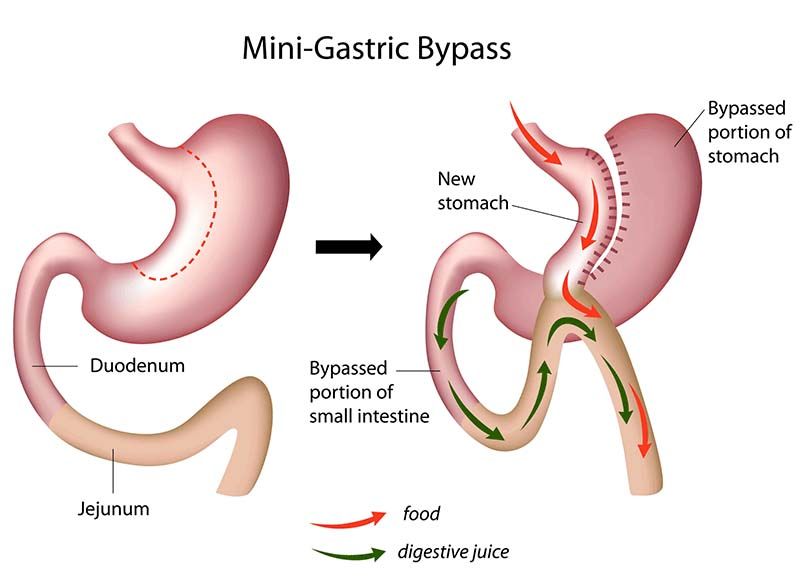
One Anastomosis Gastric Bypass
One Anstomosis Gastric Bypass (OAGB), also called Mini Bypass is a newer alternative to RYGB that uses a simplified technique with only one surgical connection (anastomosis).
How It Works:
- A long, narrow stomach pouch is created, similar in shape to a gastric sleeve
- This pouch is attached to a loop of small intestine around 150–200cm from the stomach, bypassing the upper bowel
Benefits:
- Comparable or greater weight loss than RYGB
- Shorter surgical time
- Strong improvement in diabetes and metabolic conditions
- Particularly effective for patients with high BMI or high sugar/fat intake
The Procedure:
This keyhole (laparoscopic) surgery involves creating a small, tube-shaped stomach pouch and attaching it to a loop of small intestine, bypassing around 150–200cm of bowel. It limits how much you can eat and reduces how many calories your body absorbs. With only one surgical join, the operation is simpler and often quicker than other bypass types.
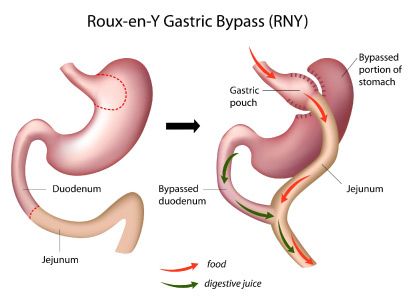
Roux-en-Y Gastric Bypass
Roux-en-Y (RYGB) is the traditional and most studied form of gastric bypass surgery. It has been used safely for decades and is considered a gold standard in metabolic and weight loss surgery.
How It Works:
- A small pouch is created at the top of the stomach using staples (around 30–50mL)
- The small intestine is divided; one part is connected to the new stomach pouch (called the Roux limb)
- The other part (carrying digestive juices) is reconnected further down the intestine, allowing enzymes and food to meet
Benefits:
- Excellent for treating severe reflux, Type 2 diabetes, and obesity-related conditions
- Long-term data supporting effectiveness and durability
- Promotes strong hormonal changes that improve metabolism and reduce hunger
The Procedure:
Performed via keyhole surgery, RYGB involves dividing the stomach to form a small pouch, which is then connected to a section of small intestine. A second join reconnects the remaining intestine so that digestive juices still flow. This creates a bypass of the stomach and first part of the intestine, reducing food intake, nutrient absorption, and improving hormone regulation.
Gastric Bypass Options: Key Differences at a Glance
| Feature | Roux-en-Y Gastric Bypass (RYGB) | One Anastomosis Gastric Bypass (OAGB) |
|---|---|---|
| Surgical Technique | Two surgical joins between stomach and bowel (more complex) | One surgical join between stomach and bowel (simpler) |
| Weight Loss | 70–80% excess weight loss in 12–18 months | 70–85% excess weight loss in 12–18 months |
| Best Suited For | People with reflux, diabetes, or needing revision surgery | People with high BMI, strong sugar/fat cravings, or diabetes |
| Hormonal Effects | Alters gut hormones to reduce hunger and improve insulin control | Strong hormonal effect for early fullness and metabolic benefit |
| Nutrient Absorption | Moderate reduction — daily supplements required | Slightly more reduction — lifelong supplements essential |
| Surgical Time | Slightly longer (due to two joins) | Slightly shorter (one join only) |
| Reflux Outcomes | Often improves existing reflux | May worsen reflux in some patients |
| Risk of Ulcers | Moderate risk | Slightly higher due to bile exposure in the stomach pouch |
Preparing for Surgery
To ensure a safe procedure and smooth recovery, there are a few important steps to complete before surgery:
- Follow a Very Low-Calorie Diet (VLCD) for 2–4 weeks prior to surgery, as advised by your dietitian
- Complete all pre-operative tests, including bloodwork and any required imaging or endoscopy
- Attend your appointments with the bariatric GP, surgeon (Telehealth consent), and dietitian
- Stop smoking at least 12 weeks before surgery and avoid anti-inflammatories or blood thinners 7 days prior
- Treat any infections (dental, bladder, bowel) before your procedure
- Arrange transport and support at home for your recovery – rural patients should plan to stay in Perth for 4 nights after hospital discharge
- Your care team will guide you through each step to ensure you're fully prepared.
What to Expect After Surgery
Most patients stay in hospital for 2–3 nights and return to normal activities within 2–4 weeks. You’ll follow a structured diet and review schedule:
- Stage 1: Liquids (2 weeks)
- Stage 2: Pureed food (2 weeks)
- Stage 3: Soft food (2 weeks)
- Stage 4: Transition to a regular, healthy diet from 6 weeks
You’ll also need to take lifelong vitamin supplements and attend regular reviews with our surgical, dietetic, and medical team to ensure success.
Long-Term Outcomes
- Average weight loss: 70–85% of excess weight
- Significant improvement or remission of:
- Type 2 diabetes
- High blood pressure
- High cholesterol
- Sleep apnoea
- Fertility and PCOS
- Improved mobility, confidence, and quality of life
Risks to Consider
Gastric bypass is safe but does carry risks, including:
- Bleeding, infection, or leak at surgical sites
- Nutritional deficiencies (iron, B12, calcium, folate)
- Dumping syndrome (rapid emptying of sugary or fatty foods)
- Ulcers or internal hernia
- Bowel obstruction or adhesions
- Rare risk of anastomotic stricture (narrowing of the join)
These risks are minimised with expert surgical care and close follow-up.
Why Choose Aurora?
At Aurora Bariatrics, your care doesn’t stop at surgery. We offer:
- A thorough, personalised pre-op assessment
- A dedicated bariatric team including Perth's leading Bariatric Surgeon, access to Bariatric GPs, Dietitian, Nurse Practitioner and Psychologist.
- Aurora's After Care Program - after surgery, you're not alone. You have access to 12 months of ongoing support, education, and follow-up to help you achieve long-term success.
Follow-Up and Support
Your journey doesn’t end after surgery — it’s just the beginning. At Aurora Bariatrics, we’re committed to supporting you through every stage of recovery and beyond.
Our 12-month After Care Program is designed to monitor your health, track your progress, and provide the guidance you need to achieve long-term success. All medical post-operative appointments listed below are included as part of your Bariatric Management Fee.
Whats Included?
| Timeline | Appointment Type | With Whom |
|---|---|---|
| 1 week | Post-op Check | Nurse Practitioner |
| 3 weeks | Surgeon Review | Dr Ruth Blackham |
| 6 weeks | Follow up | Nurse Practitioner |
| 3 months | Bariatric Review | Bariatric GP |
| 6 months | Progress Review | Bariatric GP |
| 7-11 months | SleevePlus (Optional) | Bariatric GP |
| 12 months | Annual Check-in | Nurse Practitioner |
Take the First Step
Still unsure which procedure is right for you?
Book a consultation with our team to explore your options, learn more about each surgery, and find the solution that best suits your health and lifestyle.
We're here for you!


