Gastric Sleeve Surgery
What is Gastric Sleeve Surgery?
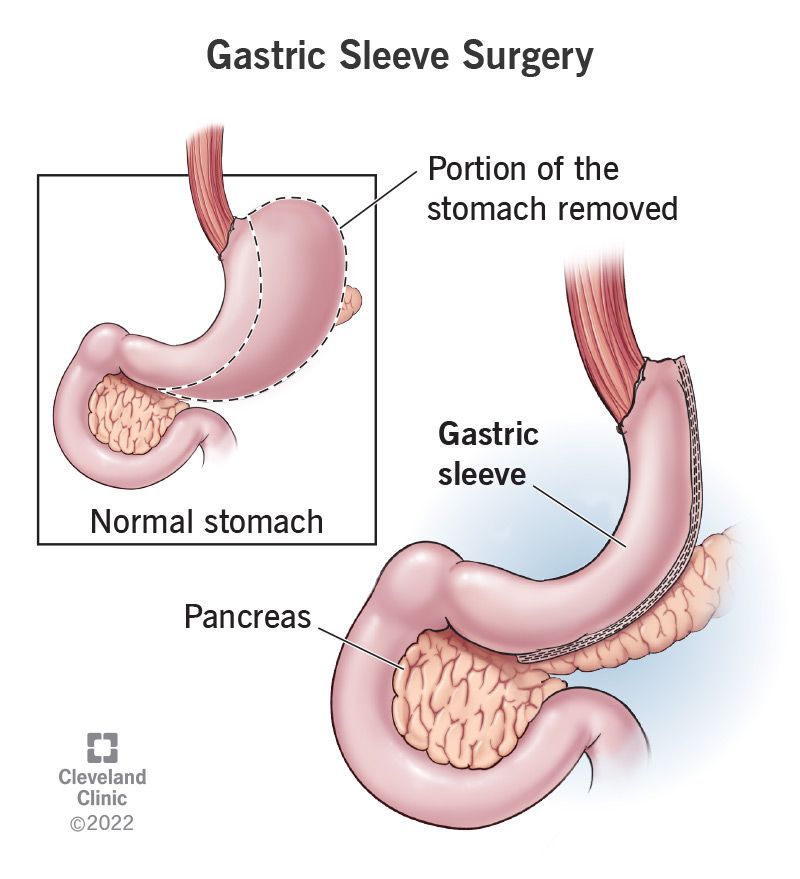
Gastric Sleeve Surgery, also known as Sleeve Gastrectomy, is the most commonly performed bariatric surgery in Australia and worldwide. It is a minimally invasive (laparoscopic) procedure where approximately 70-80% of the stomach is removed, leaving a small, tube-like stomach or “sleeve.” This significantly reduces the volume of food you can consume and influences hormones involved in appetite and metabolism—most notably reducing the hunger hormone, ghrelin.
Who Is It For?
This procedure may be suitable if you:
- Have a Body Mass Index (BMI) over 35, or over 30 with obesity-related conditions such as Type 2 Diabetes or hypertension
- Have not undergone previous stomach or bariatric surgeries
- Do not have severe reflux or other contraindications
Expected Weight Loss
Most patients can expect to lose between 65% and 75% of their excess weight within 12 to 18 months following surgery. Weight loss typically occurs at a rate of 0.5 to 2 kilograms per week. Results depend on your commitment to recommended dietary, lifestyle, and activity changes.
Benefits of Gastric Sleeve Surgery
- Rapid, long-term weight loss similar to gastric bypass
- Improvements or resolution of obesity-related conditions (e.g., Type 2 diabetes, sleep apnoea, hypertension)
- Reduced appetite and improved satiety
- Minimally invasive procedure with smaller incisions and faster recovery
- Does not involve intestinal rerouting or foreign devices
- Lower risk of nutritional deficiencies compared to bypass
Risks and Considerations
As with any surgery, there are risks. Potential complications include:
- Bleeding or infection
- Leakage from staple line (rare)
- Reflux or worsening of pre-existing reflux
- Vitamin and mineral deficiencies (managed with lifelong supplements)
- Irreversibility – once removed, the stomach cannot be restored
- Sleeve stretching over time if post-operative guidelines are not followed
Preparing for Surgery
To ensure a safe procedure and smooth recovery, there are a few important steps to complete before surgery:
- Follow a Very Low-Calorie Diet (VLCD) for 2–4 weeks prior to surgery, as advised by your dietitian
- Complete all pre-operative tests, including bloodwork and any required imaging or endoscopy
- Attend your appointments with the bariatric GP, surgeon (telehealth consent), and dietitian
- Stop smoking or vaping at least 12 weeks before surgery and avoid anti-inflammatories or blood thinners 7 days prior
- Treat any infections (dental, bladder, bowel) before your procedure
- Arrange transport and support at home for your recovery – regional patients should plan to stay in Perth for 4 nights after hospital discharge
- Your care team will guide you through each step to ensure you're fully prepared.
The Procedure
The surgery promotes weight loss in two primary ways:
- Restriction: The smaller stomach capacity means you feel full after eating a much smaller portion of food.
- Hormonal Changes: By removing the fundus (upper part of the stomach), the source of ghrelin—the hunger hormone—is significantly reduced, decreasing appetite and improving blood sugar control.
Gastric sleeve surgery is performed under general anaesthesia using keyhole (laparoscopic) techniques, which means fewer scars and faster recovery.
Here's what happens during the operation:
- Several small incisions are made in your abdomen.
- A laparoscope (a tiny camera) is inserted, providing visuals on a monitor.
- Surgical instruments are inserted to carefully divide and remove 70–80% of the stomach, including the fundus and greater curvature.
- The remaining portion of the stomach is shaped into a narrow sleeve or tube using a surgical stapler.
- The new stomach is sealed internally with staples, and external incisions are closed with dissolvable sutures.
This transformation reduces stomach capacity to approximately 100–150ml and leads to dramatic improvements in hunger control, insulin sensitivity, and overall metabolism. Because no intestinal rerouting is involved, the digestive process remains largely intact.
Recovery Timeline
- Day of surgery: Begin walking as soon as possible to reduce blood clot risk
- Week 1–2: Liquid diet; minimal discomfort; most patients manage with paracetamol
- Week 3–4: Puréed foods; gentle walking encouraged
- Week 5–6: Soft solids; return to light duties and work
- After 6 weeks: Normal diet resumed; full exercise and swimming
You must:
- Eat slowly and chew thoroughly
- Avoid drinking fluids with meals
- Take prescribed multivitamins and supplements lifelong
- Have regular blood tests to monitor nutritional levels
Follow-Up and Support
Your journey doesn’t end after surgery — it’s just the beginning. At Aurora Bariatrics, we’re committed to supporting you through every stage of recovery and beyond.
Our 12-month After Care Program is designed to monitor your health, track your progress, and provide the guidance you need to achieve long-term success. All medical post-operative appointments listed below are included as part of your Bariatric Management Fee.
Whats Included?
| Timeline | Appointment Type | With Whom |
|---|---|---|
| 1 week | Post-op Check | Nurse Practitioner |
| 3 weeks | Surgeon Review | Dr Ruth Blackham |
| 6 weeks | Follow up | Nurse Practitioner |
| 3 months | Bariatric Review | Bariatric GP |
| 6 months | Progress Review | Bariatric GP |
| 7-11 months | SleevePlus (Optional) | Bariatric GP |
| 12 months | Annual Check-in | Nurse Practitioner |
Why Choose Aurora?
At Aurora Bariatrics, your care doesn’t stop at surgery. We offer:
- A thorough, personalised pre-op assessment
- A dedicated bariatric team including Perth's leading Bariatric Surgeon, access to Bariatric GPs, Dietitian, Nurse Practitioner and Psychologist.
- Aurora's After Care Program - after surgery, you're not alone. You have access to 12 months of ongoing support, education, and follow-up to help you achieve long-term success.
Take the First Step
Still unsure which procedure is right for you?
Book a consultation with our team to explore your options, learn more about each surgery, and find the solution that best suits your health and lifestyle.
We're here for you!


